When this blog was begun, the technique of hair restoration had not advanced as it is today (September 2020) though the subject was briefly mentioned. The chapter is therefore added subsequently.
6A. HAIR RESTORATION FOR MALE PATTERN BALDNESS
INTRODUCTION
The surgical technique for restoration of living hair particularly for male pattern baldness has gained considerable traction in India over the last twenty years. When this blog was begun almost ten years ago a perfunctory entry on the subject was made in the blog in the chapters on skin grafts. However as the work in this field has increased exponentially it was thought that a full chapter needs to be written on this subject and therefore Dr. Anand Joshi a plastic surgeon from the city of Thane in the state of Maharashtra in India who has a large volume of work in this field was requested to write this chapter. The compiler of these short notes thanks him for his efforts. This chapter is mainly devoted to the treatment of male pattern baldness with small notes at the end on the treatment of loss of hair in females and loss of hair following burns trauma and other assorted causes.
This chapter is divided in the following sections:
- History
- Basic anatomy and physiology of hair and their relation to the scalp.
- Male pattern baldness – Patho-physiology.
- Classification and grading of “pattern baldness”.
- Principles of hair restoration – medical and surgical.
- Strip technique FUT – Method, limitations and complications.
- FUE technique – Method, limitations and complications.
- Combination technique – Giga sessions
- Body hair transplantation.
- Contraindications of hair restoration.
1. History of Hair Transplantation
The fact that many men lose their hair as age advances particularly from the forehead backwards mainly on the lateral side and over the vault (called male pattern baldness) has been observed over the millennia. In modern times this has been termed as androgenetic alopecia because women in the vast majority appear to be immune to this condition. While wigs have been used for centuries the history of surgical restoration of hair straddles only the last two centuries as well as the twenty first century in which the hair from the occipital area which are rarely lost even in severe forms of male pattern baldness are used for restoration of the hair population in the alopecic area.
In the early years of the 19th century Professor Unger of Germany attempted to treat hair loss by pulling out hair from the hairy part of the head and transplanting them on the non- hairy part of the scalp. But as expected the results were disappointing because he was transferring a non-living keratinous structure. However, by the end of that century hair bearing skin was being grafted and flaps from hair bearing areas were being locally transposed to treat bald areas.
More and perhaps real progress in the field began in the early twentieth surgery when Dr Okuda from Japan in the 1930s used a punch to harvest multiple hair follicles in one go and transplanted them by making holes also with a punch in an area of alopecia following burns. A Japanese dermatologist was to soon modify the technique by reducing the size of the punch which would harvest not more than four or five hair follicles and perhaps improving the chances of the “take” of the graft. But the Second World War was soon to begin and therefore the progress in this field came to a halt.
In the USA by 1952, a landmark concept of donor and recipient area dominance and their relationship in successful hair restoration surgeries was shown by Dr. Norman Orentreich. He showed that successful surgery depended on the donor being more dominant than the recipient. He showed that the follicles in the donor area are resistant to the genetic hormonal sensitivity as compared to the area involved in the hair loss where the follicles are susceptible to the circulating hormone DHT (Dihydrotestosterone). This lack of genetic sensitivity to the hormone in the donor area was termed as donor dominance because that area resisted the effects of hormones. This enlightening study was finally published in 1959. By that time other American studies also showed that baldness was an inherited condition that could be treated with hair transplants for restoration. Following a study of the areas of donor dominance, it was concluded that transplanted hair would continue to retain the characteristics of the hair from where it was taken.
The large grafts used during the 1970s came to be known as hair plugs. The results that were seen following these large punch grafts by Orentreich using Okuda’s method were unsatisfactory and not so pleasing and therefore they came to be known as ‘doll’s head look’. This technique gradually faded away and later the technique became more refined using Tamura’s smaller punch method which became the basis of modern hair restoration.
Around this time and later Scandinavian surgeons resorted to serial excisions of alopecic parts of the scalp to reduce their area and also used flaps from hair bearing skin and rotated and\or transposed them into the alopecic areas. They also took recourse to using tissue expanders both to raise flaps as well as to reduce the alopecic patches. The results however were not satisfactory.
But these techniques certainly laid the foundations for modern surgical practices that focus on safety as well as natural looking results. The dissatisfaction with these results prompted surgeons to take very small punch grafts and this effort was greatly helped by the introduction of operating microscopes. Gradually moving away from easily detectable ugly plug transplants, advances in microsurgical techniques resulted finally in micro hair punch grafting.
By 1984, smaller and smaller grafts were being used resulting in a more natural look. Micro-grafts were surely an improvement but still not perfect. By 1994, the concept of follicular unit transplantation (F.U.T.) was put forth by Drs. Bernstein and Rassman based on the dissection technique of Dr. Bobby Limmer. They used follicular units harvested from a donor strip excised from the occipital area for much better results but this procedure required more time and a certain surgical skill.
By the end of twentieth century, FUT (Follicular Unit Transfer) from occipital scalp strips was the preferred method of hair restoration. The use of a very large number of mini-micro grafts ranging upto 2000-2500 grafts for extensive areas became very common after Dr. Carlos Uebel from Brazil presented his work on extensive FUTs. Prof Uebel deserves the title of being called the father of modern FUT hair restoration.
During this era hair transplants were also coupled with medications like Minoxidil and Propecia in order to delay the male pattern hair loss and for thickening of the existing hair. In the past 30 years till date, major advancements have been made in the formulations of these medications for delaying hair loss.
Dr. Orentreich’s original idea of harvesting grafts directly from the back of the scalp, rather than harvesting a donor strip for that purpose was never really given up even though FUT was the procedure of choice for most surgeons. An Australian doctor (name not known) began to investigate the idea of removing individual follicular units directly from the donor area using a very tiny punch. In 2002, Bernstein and Rassman developed their own micro-punch and first published their work in medical literature on FUE (Follicle Unit Extraction) and then transplanting these follicles by way of minimally invasive surgery for hair restoration.
Like FUT, FUE also faced initial resistance due to a new set of surgical skills required by the surgeon as well as the assisting staff. Also, since FUE required a special device to extract whole follicular units without damage and implanting them accurately without damage, the race to develop optimal instrumentation was on. But what spurred the practice of this technique was a demand by the patients who wanted to avoid a linear scar in the occipital area.
FUE hair transplantation later gained further momentum and popularity with Dr. James Harris’ paper in 2005, in which a two- step sharp and dull punch instrument was described to minimize follicular damage during their harvest. The first step used a sharp punch to cut through till the upper dermis and then the second step used the dull punch below the dermis to prevent damage to the bulbs of the follicles.
Since then till date, technology has been evolving with newer designs of the punch that is used and motorized machinery to minimize graft loss and optimize results. The Safe Scribe or the ‘Neo-graft’ etc. are examples of such FUE automated systems. Simultaneously, Dr. Choi from Korea has now patented his “pen implanters” for implantation of grafts with minimal damage.
The latest in the hair transplant market is the ARTAS robotic hair transplantation system which has a fully automated mechanism for harvesting grafts and their implantation.
The popularity of hair transplantation by the FUE technique has increased exponentially in recent years, although FUT is still widely practiced though not preferred by both patients and surgeons. Both methods have their advantages and disadvantages or limitations for different patients, so the choice of the best possible procedure for an individual patient is certainly based on a detailed discussion with the patient considering his demands as also depending on the ability of the surgeon to fulfil them. Also, in cases of extensive baldness, a combination involving both the FUT and FUE procedures has been used lately to give maximum coverage by harvesting a larger number of grafts in a single session. These are termed as ‘giga sessions’ of over 3500 follicular unit grafts.
Also recently extensive research has been going on in transplanting hair from other parts of the body to the scalp in cases where there is a paucity of scalp donor hair such as in in very high grades of androgenetic alopecia and also in those cases where the scalp donor area has been completely exhausted due to multiple sessions of hair transplants done earlier. Nevertheless, the principle of “donor dominance” still holds true and these transplanted hair from other parts of the body have not been found to change their original genetic characteristics and therefore do not produce satisfactory results.
What perhaps lies in the future is cloning and genetic engineering in which hair follicles will be grown from stem cells in large numbers which then can be transplanted with great ease without the need for a harvest from a donor area
FUT (Follicle Unit Transplantation) and FUE (Follicle Unit Extraction) are short forms which will be used in the following sections.
2. Basic anatomy of hair
The embryological origin of hair is both ectodermal and mesodermal.
The keratinous hair and pilo-sebaceous follicle are ectodermal in origin and the dermal papilla is of mesodermal origin.
Hair consists of a shaft and a root. The shaft is the visible portion above the surface of the body. The root or the bulb is the follicle and is placed at a specific angle in the dermis. This angle varies from one area to the other.
The shaft has three layers from the external to the internal, cuticle, cortex and medulla.

The entire shaft consists only of keratinised cells which contain keratin, a fibrous protein produced by the hair follicle. This keratin is an end product of the hair matrix which exists at the base of the hair follicle in the subcutaneous tissue. The matrix has rapidly dividing cells and above this is the zone of keratinization which gets transformed into the ‘hair shaft’ as it exits the follicle above the skin surface.
The constant layering of these newly keratinized cells at the bottom of the shaft causes the process of hair growth and the shaft gradually moves up through the follicle beyond the surface of the skin.
The average rate of growth of any terminal hair on the scalp is approximately 0.3 to 0.4 mm per day or 1 to 1.2 cm per month.
Types of hair:
There are basically two types of normal adult hair, the vellus hair and the terminal hair. Vellus hair is short, soft and hypopigmented hair that can be almost invisible, found over the entire body. Terminal hair is long, coarse and pigmented and are present over the entire scalp, eyebrows, pubic and axillary areas, as well as in the beard and the moustache.
Average diameter of the scalp and beard hair is 60 to 100 micro-meters.
The colour and hair diameter vary considerably in different races. Whites have thinner and lighter or blonde hair whereas blacks and Asians have thicker dark black or brown hair.
The shape of hair also varies greatly. Wavy hair is more oval in cross section as against stiff or straight hair which are rounder on cross section.
Another important variable is the density of hair per square cm of the scalp. It varies from as high as 200 in the Caucasians to even lower than 60 to 80 hair follicles per square cm in Africans. The average Indian hair density is 100 to 150 hair follicles per square cm.
Follicles on the scalp always exist as groups of 2, 3 or 4 hair follicles clumped together called as follicle units also termed as pilosebaceous units. Every follicle has its individual sebaceous gland secreting oil or sebum which acts as nourishment for the hair and also its individual capillary network and a nerve plexus in the subcutaneous tissue and deep dermis for its blood and nerve supply. That is why every hair root is always sensate and hence any pull on the hair gives rise to pain at the level of the root. Every hair follicle also has its own erector-pilae muscle which has an autonomic nerve supply responsible for erection of the hair in certain reflexes which is a part of a protective evolutionary process inherited from lower animals.
Anatomy of a normal hairline:
An important characteristic of a natural hairline is the transition from fine, single scarcer hair to denser and thicker hair with a fair degree of irregularity along the margin. No hairline is perfectly straight, it always has a staggered pattern throughout its entire length.
In young men and women there is no frontotemporal recession whereas the critical anatomical landmark in a mature male hairline is marked by a frontotemporal recession.
This anatomy of the hairline is very important while planning the post treatment hairline in any hair restoration. In the front a 3 to 4 mm zone always consists of sparser hyper acutely placed fine single hair beyond which thicker follicle units are densely packed to give the most natural appearance during hair restoration.
Physiology:
Phases of hair growth also called the hair cycle. There are essentially three phases of hair growth. Anagen, the first phase is the active growth phase lasting for 2 to 6 years with some variation. During this period, the follicular cells are actively dividing and hair grows in length. This is followed by the catagen also called the involution or regression phase in which there is degeneration of keratinocytes and special mesenchymal cells and they gradually cluster and separate from the dermal papilla. This phase lasts for 2 to 3 weeks. The final resting phase called telogen lasts about 3 to 4 months during which the follicle is inactive and hair growth ceases. The dermal papilla gradually releases from its epidermal attachment and there is reformation of a growing bulb. The old hair gets shed and then a new hair starts growing through the newly formed papilla thereby again entering into the anagen phase of growth.
When hair are restored by implantation, the mandatory waiting time required for hair growth after follicle implantation is due to this telogen phase of rest. As soon as the hair follicles are harvested from the body, they lose their blood supply and immediately enter into the telogen phase of fall and rest. Once the implanted follicle is revascularized and this occurs from the sides of the implanted follicle unit which carries a thin layer of connective tissue, it once again enters into the anagen phase and then the hair starts growing. So visible hair growth after hair follicle implantation is seen only after a 12 to 16 weeks called the “waiting time.”
3. Male pattern baldness: Pathophysiology
Male pattern baldness is scientifically termed as androgenetic alopecia. The typical process of male balding pattern is a gradual thinning and receding of hair starting from the temporoparietal hairline, generally after 22 to 25 years of age, then gradual involution of the frontal hairline over the crown and then lastly followed by receding of the vertex hair. In some of the cases or in the case of familial pattern baldness, this receding may start initially in the vertex area and then gradually spread in the front towards the hairline leading to a “reverse pattern of baldness”. Finally, after the entire recession of the hair in the frontal, crown and vertex zones, a horse shoe shaped area of the permanent hair remain intact over the occipital and parietal scalp without any thinning or involution. This area is termed the donor zone of permanent hair.
Baldness is a gradual process in which the hair starts thinning and finally disappears. Actually what happens is that a good terminal hair gradually thins out and gets converted into an involuted vellus hair and finally is not visible to the eye due to its fineness and hypopigmentation. So, baldness doesn’t mean disappearance of hair follicles, but it means gradual conversion of terminal hair into vellus hair starting from the front to the vertex or vice-versa. Every follicle in the bald area exists but cannot produce a terminal hair because of the binding effect of testosterone on the terminal follicles shunting their growth in the anagen phase, gradually reducing the hair diameter and leading to early stimulation of the telogen phase.
The mode of action of androgens on the target cells occurs at the bulbar region of the follicle. Testosterone is converted into dihydrotestosterone (DHT) by 5 alpha reductase. DHT then acts on the target cells at the dermal papilla and shunts the “hair growth”. This sensitivity of follicle cells to DHT is genetically determined and is under the control of a single dominant sex-linked autosomal gene.
However, it is believed that this may be influenced by other modifying factors and there is probably a polygenic component to the expression of male pattern hair loss.
One thing is very clear that the expression of these genes rarely occurs before 20 years of age. Generally, all patterns are seen to start after the age of 22 to 25 and gradually these patterns proceed to the final grade by the age of 40 to 45. In some families, delayed patterns of male baldness are seen to start after the age of 45 to 50 years.
Another variation of a balding pattern is where there is only an overall thinning pattern in the entire zone from the frontal up-to the vertex without actual hair loss, which means only some hair go into involution and turn into vellus hair and some remain as terminal hair giving rise to a typical appearance of loss of density alone as compared to the other patterns.
4. Classification and grading of androgenetic alopecia
Types of male pattern baldness:
- A predominantly frontal pattern with intact vertex
- A Predominantly vertex pattern with intact frontal hairline
- A Frontal and vertex pattern with intact mid zone.
- A Full pattern from front up-to the vertex
- A Generalized thinning and a pattern marked by loss of density
Many classifications exist and have been described on a morphological basis comparing the hair bearing scalp with the non- hair bearing scalp areas. The first classification of baldness patterns was put forth by Beck in early nineteenth century followed by Hamilton in 1951. He analysed hair loss patterns in both whites and Chinese population.
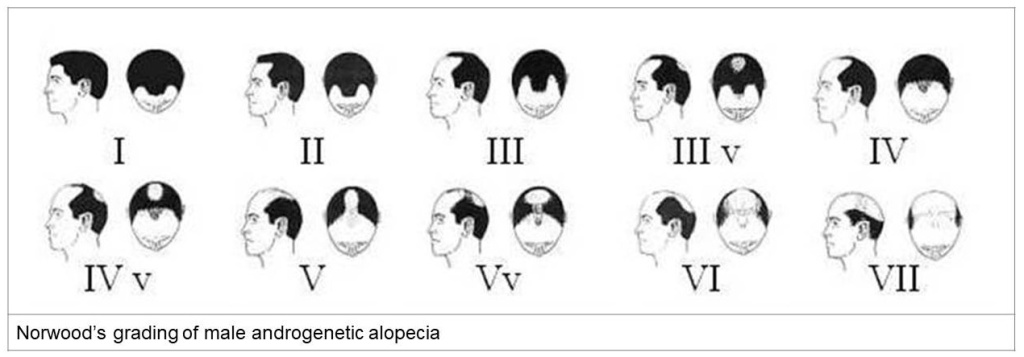
Later Norwood modified Hamilton’s classification into a grading system from grade 1 to grade 7.
Grade 1, 2 and 3A are patterns with only temporal receding in an increasing order. Grade 3B is when it is pattern 3A with vertex hair loss.
Grade 4 and 5 are advanced patterns of 3B in an increasing order
Grade 6 is a full frontal to vertex pattern hair loss
Grade 7 is advanced 6th grade with a very limited horse shoe donor area
Another classification system was put forth by Bouhanna and Dardour which distinguishes three stages with variances in stage 1 and stage 2, thus defining 5 basic patterns.
Out of all these, Norwood’s classification is the most widely accepted grading system all over the world.
Ludwig devised a classification system for density loss patterns especially female patterns of hair loss. He divided them into three grades 1, 2 and 3 depending on severity of density loss and area of thinning.
5. Principles of Hair Transplantation
Hair transplantation is not a transplant in its true sense. Any transplant in its true scientific sense is transfer of any organ from one body to another. These organ transplants are now quite common but carry the added burden of immune suppression to prevent rejection. Immune suppression is known to carry a certain risk and it is often said that this risk is taken to give new life to an individual. In front of this backdrop homologous hair transplantation has not been encouraged or practiced because the indication for hair restoration are purely aesthetic and the condition of primary alopecia is not life threatening.
The first principle therefore of hair transplant is that the patient is his own donor. It is in the strictest true sense micro hair grafting or transfer of hair follicles from an area of abundance which is called donor zone to the area of loss of hair or deficiency.
The second principle of surgical hair restoration is the principle of donor dominance which means that hair from any area on the body retain their genetic characteristics even after grafting onto any other area. So, when occipital area hair follicles are harvested and grafted into the frontal or vertex areas of hair loss, they are not affected by the DHT sensitivity of follicles in these areas of androgenetic hair loss. After transplantation these follicles retain the donor characteristics and continue to grow terminal hair for a life time without miniaturization. Therefore, due to this retention of donor dominant characteristics, hair transplantation is a permanent restorative procedure requiring no medical maintenance.
The third and last principle of hair transplantation is that there is a limited supply of donor hair. The total number of hair follicles on the entire body is always constant and cannot multiply or increase by way of any intervention. By a rider after androgenetic alopecia progresses to the final grade, whatever donor area left over has finite number of hair follicles which are approximately less than one fourth of the follicles on the total scalp area. So, on an average approximately 20 to 25 thousand follicles are left over in the possible donor area. Out of these less than 50% are available for harvest in multiple sessions. The maximum number of follicles that can be harvested at one given time or in a single session cannot exceed 20% of the total available follicles.
So practically in a hair transplant procedure, the hair restoration surgeon is trying to create an illusion of a full head of hair using a far fewer number of hair follicles using his artistic sense to achieve the maximum possible restoration. No hair transplant can give normal or near normal density in the transplanted area simply because of this limited availability of donor follicles and even after multiple sessions density cannot be normalized simply because the number of transplanted units can never match the original number of hair which are lost by the process of androgenetic alopecia.
6. Strip Method of Hair Transplantation
Strip technique of hair restoration is also commonly called the FUT hair transplant. By this method, a full strip of occipital scalp skin is marked and harvested as per the requirement of grafts depending on the coverage area targeted.
The width of the scalp strip can be up to a maximum of 1.75 cm or in some cases with excellent scalp laxity, we can harvest up to 2 cm width. Length of the strip depends on the number of grafts required for the target area. In higher grades, the maximum length of the strip that can be harvested from one temporal area to the other can be anywhere from 20 to 25 cm of length. So, with an average density of around 100 follicle units per square centimetre, we can get about 2000 up to 2500 follicle unit grafts from such a “full scalp” strip. Very rarely with excellent donor density, we can get up to 3000 follicle unit grafts for restoration.
After harvest of the scalp strip, the defect must be closed in two layers without undermining of the scalp skin.
Once the entire length of scalp strip is harvested, the surgeon divides this strip into multiple vertical slivers of single or double follicle units depending on the density of follicles. This slivering is always best done under a good magnification minimum of 4X to avoid transaction of follicles during slivering. This is the most important step of a strip hair transplant.
Once these thin slivers are cut from the entire strip, individual follicle unit grafts are separated from every sliver by the trained assistants again using magnification level of minimum of 2X to avoid transaction of individual follicles. Both these steps of slivering and graft separation are essentially done on wooden strips or boards embedded in normal saline to avoid desiccation of the follicle grafts.
These separated slivers and follicle unit grafts are stored either in glass petri- dishes filled with lactated ringers solution or in plain plasma to avoid desiccation and these dishes are always kept over ice packs to maintain the temperature of the harvested tissue to less than 10 degree centigrade, ideally at 4 degrees to reduce tissue metabolism and thus increasing the graft survival time outside the body.
The separated follicle unit grafts are finally inserted in the recipient scalp by the technique of one “slit one graft” till the entire target area is covered by the available harvested grafts. Slits can be made either using 18, 19 or 20 gauge needles or using 11 number surgical blades or by the cataract knife as per the choice of the operating surgeon.
There are distinctly two methods of graft implantation, one is the pre slit method where all the slits or needle holes are made before implantation of grafts and the other is the slit and place method where a graft is implanted as soon as the slit is made. Method of implantation is again as per the surgeon’s choice. Generally, slit and place method is the preferred method of surgeons who operate and do the implantation by themselves whereas the pre-slit method is used widely by a majority of surgeons who employ technicians for implantation of grafts. The slit and place method is certainly more difficult to master and has a very long learning curve. Moreover, only the surgeon can do the implantation and hence it takes a longer time and at the same time is physically tiring as well. As against this the pre slit method proves faster as more than one technician can work on the field after the slits have been made, and also in turn avoids surgeon fatigue. Generally plastic surgeons do not prefer this method as they operate by themselves but it is widely used by dermatologists who employ technicians for implantation. The biggest disadvantage of a “technician based team” is that there is no control over tissue handling and graft damage due to crush injury by the graft holding instruments as the surgeon is not involved in the procedure.
Whatever be the method of implantation, the direction and angulation of the slits has to correspond to the original direction of slits in the area of implantation to produce a natural look after “hair growth”. So, the naturality in the look of transplanted hair is directly proportional to the operating surgeon’s surgical skill.
Advantages of strip method:
- Scalp strip can be harvested without trimming or shaving of the entire donor zone. Only the strip area to be harvested can be trimmed or shaved and the rest of the scalp with long hair is left untouched. Once the strip is cut and harvested, the left over long hair are available to cover the wound and the sutured area. Hence the cut and the sutured wound in the donor area remain hidden as they are covered with long hair.
- As no trimming and shaving of scalp is necessary, the patient always retains his primary look after the surgery.
- The strip is always harvested from the best zone of the donor scalp so the best of the follicles are available for grafting and results are therefore optimum.
- The donor area above and below the harvested strip zone remains essentially normal with normal hair density and hence is available for a second graft harvest. As a result, any future session has areas available for a future harvest when the first session is done by the strip method.
- After a strip harvest, every follicle unit is under direct vision under magnification and therefore there is minimal chance of follicle transection during slivering and graft separation. So, there is a minimum loss of harvested follicles in the strip method.





Disadvantages of the strip method:
- As there is a long cut and stitching is required for closure the pain of the procedure persists for a few days after the effects of local anaesthesia wanes off and supplementary analgesics are needed and antibiotics may need to be given.
- The long cut always leaves a permanent linear scar in the occipital scalp which is easily visible in the hairy scalp when the hair is trimmed short or shaved
- In mega sessions for advanced grades of baldness, the strip always gives limited number of grafts depending on the follicle density per square centimetre of scalp as wider strips cannot be harvested due to limitation of scalp laxity and difficulty in closure in wide strips.
- The stitches used to close the donor area need to be removed. So, the patient has to follow up after 10-12 days for suture removal. In some selected cases, where the patient cannot follow up for suture removal, there is an option to use absorbable sutures and total subcuticular closure but generally not preferred for fear of hypertrophy of scars
7. FUE Method of Hair Transplantation
FUE is follicle unit extraction method in which every individual follicle unit is harvested directly and separately from the scalp by a micro punch varying in size from 0.6mm to 1.2 mm depending on the circumference of the follicle. Most commonly used punches are 0.8, 0.9 1 mm. Punches narrower than 0.8 mm tend to damage the follicular tissue and wider than 1 mm tend to damage the surrounding follicles and so are not preferred. The idea is to get one follicle with enough soft tissue around it to help vascularisation.
In this method of graft harvest, individual follicle units are harvested from a larger donor area separately and in a random manner leaving behind a good number of follicle units around every harvested follicle unit. So, this method of graft harvest essentially leads to reduction of follicle unit density of the donor area.
The extraction is not limited to a concentrated area of the donor as compared to the strip method where all the follicles in the strip area are harvested for transfer and therefore a much wider donor area of hair needs to be trimmed or shaved for follicle harvest. Random extraction can be done from the entire donor zone that is available.
Generally, the harvest of follicles in FUE should not exceed more than 20% of the actual density per square cm of the scalp in one session of graft harvest. So as a general rule, with an average density of 100 units per square cm, the harvest of follicles should not exceed 15-20 units per square cm. Exceeding this limit of harvest may give more number of grafts but in turn can lead to depletion of donor density and damage to left over existing follicles due to excessive scarring in the process of healing.
The most important point to be understood here is that every follicle unit that is punched out is going to be replaced by an individual dot like scar. So, all the individual scattered punches are going to be replaced by innumerable permanent dot like scars scattered everywhere in the donor area. These scars would be certainly visible only if the donor area is trimmed or shaved but cannot be easily visible with grown longer hair.
The methods of storage of harvested grafts and also the implantation that follows are essentially the same as that of the strip method mentioned earlier. So logically and practically the results of hair growth produced after one year are similar for both the methods of hair transplantation. The difference in these two methods is essentially in the method of graft harvest, the method of implantation remaining the same.
Advantages of FUE method:
In the absence of an incision and its subsequent closure the pain that results following the FUE method is considerably less and so is the use of analgesics.
- As there is no limitation on the width of donor area, the entire donor zone is available for graft harvest and hence for higher grades of baldness patterns, a comparatively larger number of grafts can be harvested from the entire donor zone for coverage. A maximum width and length of an average scalp strip cannot give beyond 2500 follicle units but an entire donor zone in the FUE method can give up to 3000 or more grafts in a single harvest session.
- The scars produced by the FUE method being scattered dot like scars they are not easily identifiable from a distance even in a shaven head or trimmed hair as compared to the linear scar of the strip which may be visibly identifiable even from a distance. So FUE scars are aesthetically more pleasing than the scar in the strip method.




Disadvantages of FUE method:
- Large donor area needs to be trimmed or shaved for the FUE harvest so the patient generally prefers a full head trim or shave which becomes necessary. FUE harvest can’t be done with long hair and therefore the patient must compromise on the way he looks for some time till the hair grow back as compared to the strip method where little shaving needs to be done and the patient retains his earlier look.
- FUE harvest takes a longer time and hence mega sessions of over 2000 grafts need to done divided over 2 or 3 consecutive days depending on graft harvest and area of coverage. So, the surgical operative time is more as against the strip method which is essentially a single day procedure.
- FUE graft harvest produces randomly scattered dot like scars in the donor area reducing the overall donor density and therefore the subsequent availability of follicles for a second session harvest reduces significantly. Moreover, due to the scattered scarring, the harvest of follicles adjacent to these scars is technically more demanding with higher chances of follicle graft transections. Comparatively in the strip method, the remnant donor area adjacent to the linear scar is virgin with normal follicle density for follicle harvest in further sessions.
- Punched follicles are always thinner in calibre as compared to strip harvested grafts as there is abundance of surrounding tissue in strip grafts. So, strip grafts are more robust and easier to handle with less chances of “crush damage” due to abundance of tissue around the follicle. As against this FUE grafts lack adequate tissue around the follicles and hence are more prone to crush injury in handling during implantation.
- The last but most important disadvantage of the FUE method is that it is a blind procedure of graft harvest. During the process of punching, only the hair exiting the scalp skin is visible. The bulbs are not visible from the surface. So, the intact follicles need to be harvested with utmost skill taking into consideration the angle and the direction of the follicle placed in the dermis. So, no matter however skilful the operating surgeon may be, there are always chances of graft transection and follicular damage. That is why the harvest of 100% viable non-transected grafts is always questionable and there is always a chance that some follicles might get transected and on an average around 5 or 10 percent of inadvertent transection has come to be acceptable even in experienced hands. Strip graft harvest is entirely under magnified vision and therefore chances of follicular transection are far less. So, the overall percentage of hair growth in strip sessions is relatively more than the percentage growth of FUE sessions.
Techniques of punching in FUE :
FUE can be done either by manual punching methods or my motorized or automated punching methods.
Manual punching is always done by sharp punches or semi sharp punches which cut through the epidermis and upper dermis by oscillating motion of the punch induced by the pinch grasp between the thumb and fingers. The punch is aimed on the follicle unit of choice generally randomly selecting the prominent follicle units under magnified vision and the direction of the cutting punch is adjusted according to the approximate direction of the follicle by visual judgement and comparing with the adjacent follicles. Once the upper dermis is transgressed up to 2.5 to 3 mm depth a sensation of “give” is felt by the punch and the punch is immediately withdrawn. The next step is extraction of the follicle by holding it at the dermal level and pulling it out of the skin ensuring that the bulbs are completely intact. The depth of punching required depends on the length of the follicle within the dermis which is variable from person to person. Some surgeons use a “two punch” technique for the manual method. The first 2 mm up to upper dermis is cut with a sharp punch with oscillating cutting movement followed by use of a blunt punch into the deeper dermis to avoid bulbar transections.
Motorized punching is a relatively advanced technique for increasing the speed of graft harvest. Motorized FUE harvesters can again be of the oscillating type or rotational type choice to be made by the individual operating surgeon. In motorized punch harvest all three types of punches can be used, sharp, semi sharp or the blunt punches clearly depending on the individual surgeon’s choice. The RPM (rotations per minute) of the machine has to change according to the type of punch. Very sharp punches require very low RPM whereas blunt punches require a higher RPM and semi sharp ones require intermediate RPM. Sharp punches logically and practically have higher transection rates but lesser surrounding tissue injury due to a lesser RPM whereas blunt punches have lesser transection rates but more surrounding tissue injury by friction due to a higher RPM.
So, every method has an advantage as well as a disadvantage. The choice of the gadget rests clearly with the individual surgeon. No matter what technique is used, finally the harvested follicle unit should have an intact bulb, (without transection) and with sufficient follicular tissue with its surrounding soft tissue for graft survival.
Types of punches:
- Sharp punches
- Semi-sharp punches
- Dull or blunt punches
- Serrated punches
- Conical punches
- Hexagonal punches
- Inner bevelled punches
- Outer bevelled punches
- Bi-bevelled punches
Punches are also named by the surgeons who invented them e.g Harris’ punch, Cole’s punch, Ertip punch etc. Every individual surgeon has the liberty to design a punch according to his specifications and innovations to reduce graft transection.
8. Combination Technique: FUE + FUT
In very high grade androgenetic alopecia beyond grade 4-5 with a good donor area availability, the use of combination technique procedures gives significantly more number of grafts for coverage in a single session provided the patient desires so and in cases where there is lack of waiting or down time for subsequent sessions.
The main disadvantage of this combination technique is the exhaustion of the entire donor area in a single session leaving minimum possibility for further graft harvest in subsequent sessions. The other drawback of such a combination of techniques is the prolonged total operative time which makes it tiring for the patient as well as for the operating team.
The general protocol for a combination technique is to do a maximum strip session on the first day which can give up to 2000 to 2500 grafts depending on donor density followed by a maximum FUE session from the remaining donor area over the next 2 days which can give additional 2000 to 2500 grafts for further coverage. So, with a combination of strip and FUE technique, graft harvest can be maximized to 4000 follicle units or even more if donor density is excellent. These are called giga sessions.
9. Body Hair Transplantation
Donor areas other than the scalp donor zone are also available for follicle graft harvest e.g. the beard area, chest and back, abdomen, pubic and axillary hair in the order of preference. Body hair as donor follicles are used for graft harvest only after the scalp donor zone is exhausted and that no more follicle grafts can be harvested from the scalp. Body hair follicle grafts are never used for primary restoration of any area of hair loss. Body hair grafts are essentially used as fillers only for improvement of density of transplanted hair and to provide a fuller look. The most natural look can be obtained only by scalp hair. No other hair on the body can match the genetic characteristics of scalp hair in terms of texture, thickness and length. The only hair that can match the length of scalp hair are the beard hair. So, the beard is the next area of choice as a donor after the scalp.
Harvest from body hair is essentially by the FUE method as strip scars in body areas are not aesthetically acceptable and they also do not give the desired number of follicles as body hair density is far lower than scalp hair density.
Drawbacks of the harvest of body hair follicle as noted outweigh their advantages and it is therefore not a preferred method of hair restoration except in selected cases. Larger surface area of the body requires larger doses of local anaesthesia for field blocks. So, the limitation of graft harvest in one session depends on the tolerable dose of local anaesthetic. Therefore mega-sessions of body hair grafting has to be done in multiple sessions over many days.
Also, as the body skin is quite lax and soft as compared to the scalp skin harvest of follicles is technically more difficult as there is no bony support like in the skull which is available in the skin of the scalp. As a result, the rate of follicular transection is also much higher as compared to scalp grafts.
Overall body hair grafts are always available when multiple sessions are desired by the patient for an increase in the density of hair after the scalp donor area is exhausted and in rare cases where the scalp donor area is extremely scanty and body hair is available in abundance. The decision of harvesting hair from the body has to be taken judiciously by the surgeon only after adequate counselling of the patient in terms of acceptance of the final result probability of relatively un-aesthetic results due to variations in the genetic characteristics of body hair. In general body hair after transplantation on the scalp have not been found to change their original genetic characteristics.
10. Limitations and Contraindications
As is obvious hair restoration is not possible in very severe cases of hair loss such as the Norwood stage 7 where there are no hair follicles that can be transferred from the scalp and the rest of the body has paucity of hair.
The only second absolute contraindication for surgical hair restoration is in a case where the patient is not fit for a surgical procedure due to any reason from the point of view of administrating anaesthesia. Though hair transplantation is a procedure done almost always under local anaesthesia, sometimes due to cardiac insufficiency, the anaesthetist may declare the patient unfit even for such an administration. Such cases have to be perforce rejected for surgery.
Certain other medical conditions like severe diabetes or hypertension or any other medical condition may be considered as relative contraindications and the judgement rests with the treating surgeon.
Also, certain medical conditions of autoimmune hair loss like alopecia areata or alopecia totalis or dermatological conditions like cicatricial alopecia and pseudopallade are contraindications for surgical hair restoration because in these cases due to the autoimmunity factor in the loss of hair and scarring, the fate of transplanted hair follicles cannot be guaranteed.
Age is not a contraindication for hair transplantation and nor if the hair have gone grey which is an inevitability of the older age group and they too are candidates for this procedure if they are fit as long as there is abundance of hair. Surgical hair restoration can be done at any age.
Photographs of various instruments used for these procedures are shown below.




Leave a comment