30. Principles of Surgical Treatment of Craniofacial Clefts
- The first chapter in these short notes titled ‘Nature of Plastic Surgery’ used the modern expression value-addition and then explained that this addition could either be in the form of functional improvement or a structural alteration leading to a better appearance. That chapter also discussed the word ‘defect’ which is commonly associated with a “lack of something essential or required” or a shortcoming. But it also added that the word defect can be understood as a blemish or an imperfection. It follows therefore that a defect can also be in the form of an excess or a deviation from what is believed to be normal.
- In that chapter titled ‘Nature of Plastic Surgery’ the plastic surgical activity was divided into four major categories to achieve the desired results while treating defects.
- Rearranging tissue
- Substituting tissue
- Removing tissue
- And building something where nothing or very little existed before.
- It so happens that in the treatment of craniofacial clefts these four classical principles come into play individually and often are combined together for a single clinical reconstruction.
- The example of surgical treatment of hypertelorism caused by a median cranial cleft can explain this point.
- The movement of the widely separated orbits medially is an example of rearrangement of tissue as in (a) paragraph 2 above.
- This movement is possible only when the excess dysplastic tissue in the median plane is excised as in (c) paragraph 2 above.
- The medial movement of the orbit leaves defects on the lateral side which will need substitution and is filled with bone grafts as in (b) paragraph 2 above.
- And if the hypertelorism is caused by a gap in the median plane leading to meningoencephaloceles, not only does the herniated tissue need to be repositioned in the cranial cavity but the gap in the cranium needs to be bridged and the almost undeveloped bridge of the nose might need to be built with a bone graft as in (d) paragraph 2 not to mention the excision of the excess skin envelope surrounding the meningoencephalocele as in (c) paragraph 2. Please see chapter on Hypertelorism (chapter 28).
- Having said that surgeons who treat craniofacial clefts must bear in mind that some cases are untreatable in the present state of our knowledge and craft (see case 1).
All the following photographs, except Case 2 were graciously provided from the Craniofacial Surgical practice of Nitin Mokal from Mumbai. Photographs of Case 2 were provided by Rajeev Redkar, Paediatric surgeon from Mumbai.
Case 1
Perhaps some reconstruction of the ear might be possible but overall nothing significant can be achieved to improve his face.
At the other extreme reproduced below in case 2 are photographs of an innocuous looking nasal cyst which is in fact a dermoid with an intracranial origin as shown by the MRI and a probe appearing intracranially through a track leading in the superior direction from the dermoid. Gap in the nasal bone is clearly seen. The intracranial gap was closed surgically by a transcranial approach and the dermoid was also excised.
Case 2
Several examples of craniofacial clefts which have been treated are given below but they are not numbered because the treatment is not determined by the number of the cleft but by its pathological anatomy. Also because the previous chapter (29) on classification of craniofacial clefts has more than one classification and the numbers don’t match in the two classifications.
Case 3
Case 4
These two examples show an anatomical approximation of the lip including its muscles. The deformity of the nose has been self-corrected by way of the approximation and not by any surgical work on the nose itself.
Case 5
This cleft has been repaired with muscle approximation and with a Z-plasty in the skin envelope. The movement of the lip towards the midline has brought together the nasal skeleton which was symmetrical but was spaced apart. The philtral dimple is now occupied by a scar and it is likely that the dimple cannot be recreated as in a standard cleft lip repair. The lowermost picture on the right side shows a late follow up.
Case 6
This cleft mainly in the nose, also shows a mis-matched vermilion. The nose has been treated by a flying bird incision and a sequestrated dermoid like tissue at the root of the nose has been excised. The MRI did not show any gap in the cranial bone. After the dermoid was excised, lower and upper alar cartilages were mobilized to facilitate their approximation after a nasal bone osteotomy (infracture). A right angle iliac crest bone graft has been used to increase the height of the nose. The vermilion mismatch has been treated with an elliptical excision of the skin as well as the vermilion to bring together two equal cylinders of the lip for symmetry.
Case 7
Similar case as in the previous example. This case has received a costal osteocartileginous graft to the nose.
Case 8
This cleft involving the lip and the lower eyelid on the left side has been treated with multiple Z-plasties without any import of tissue. A medial canthal repair will follow.
Case 9
This cleft has been treated on the surface by multiple Z-plasties but the middle picture shows a linear streak of local skin being used for a reconstruction of the naso-lacrimal duct from the medial punctum of the left lower eyelid and was invaginated into the area of the turbinate.
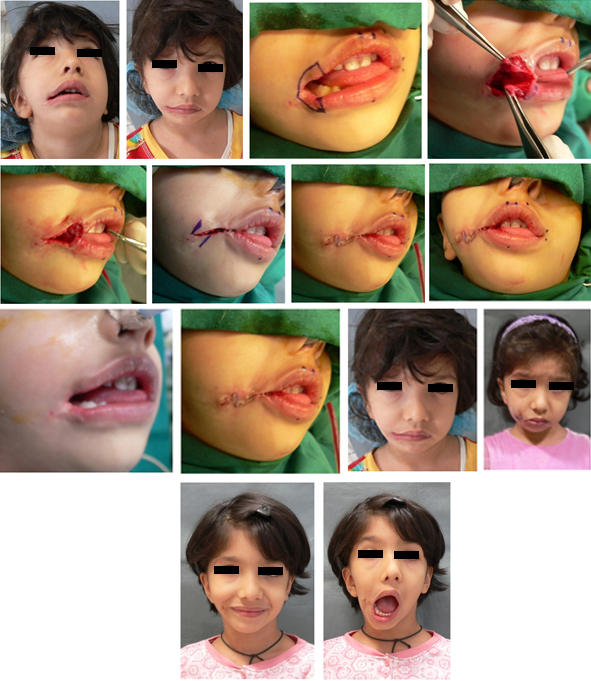
Case 10
This right lateral cleft arising from the oral commissure has been treated with approximation of the divided orbicularis oris creation of the oral sphincter and then a Z-plasty on the skin. Late post-operative results show a pleasing result and normal oral opening.
Case 11
A similar lateral cleft as in the previous example but in its more restrictive and severe form has been treated with multiple Z-plasties both on the skin as well as the mucosa in view of its intra-oral extent.
Case 12A

Case 12 A: A cleft in the nose on the frontal bone with Hypertelorism. Local alar tissue is being transposed to create a nostril.
Case 12B

Case 12 B: A forehead flap of skin based on a subcutaneous pedicle has been rotated to close the defect created by the movement of tissue used to create the nostril.
Case 12C

Case 12 C: The upper photographs show the steps so far taken. The lower two photographs show the reconstructed alar area has been defattened and the meningeal bulge in the forehead has considerably reduced because of plication of soft tissue surrounding the bony defect.
Case 12D

Case 12D: The reduction of meningeal herniation by local plication has allowed new bone formation in the frontal area (above top) and the lower photographs show surgery for hypertelorism in progress. The intraorbital distance is being measured intra-operative.
Case 12E

Case 12 E: The top two pictures show the completed orbital osteotomies. The long sutures will criss cross to effect canthal repositioning and their fixation. The middle two pictures show the reduced intraorbital distance and a cranial bone graft fixed to the frontal defect. The lower photographs show fixation of the orbits and the bone grafts to the defects created by movement of the orbits.
Case 12F
Case 13
In this cleft there is an abnormality in the eyebrow which has been corrected by a Z-plasty.
Case 14
In this bilateral cleft the lip has been radically mobilized on the left side, less so on the right side and Z-plasties have been employed from available adjacent skin to fill in the gaps. Please note that some ectropion of the lower eyelid on the left side persists and will probably need some kind of skin substitution as the child grows older. As is known because the ectropion is in the lower eyelid no adverse effects are seen in the eyeball.
Case 15
This craniofacial anomaly usually called bilateral hemifacial microsomia (which has been described in an earlier chapter) is a “non-cleft” craniofacial anomaly arising from the same embryological etiology of non-development of parts or processes which join together to form the face. The patient also has deformities of the ears which is a part of this syndrome. The mandible is severely retruded leading to poor occlusion and a very short face in the anterio-posterior dimension in the lower half. The pictures reproduced here show mandibular osteotomy (done on both sides) before distraction is begun which continues for several months. The illustration also includes x-rays to show the gap in the mandible which automatically got filled with new bone. The later pictures show the mandibular distraction having been completed the mandible now matches the maxilla with good occlusion. Reconstruction of the ear will follow.