55. Cleft Palate and Speech
- For health care professionals dealing with the treatment of children with cleft palates, good speech remains a very important outcome.
- In the past, surgeons seemed to be the sole caregivers in this speciality, leading to a ‘quote’ by Ian Jackson (Fig. 1)
 who wrote in 1983, that the main contributors that have revolutionized cleft palate surgery over the years more often than not do not contain representatives of the “speech world”. The statement riddled with a double negative, in plain words, points out that speech pathologists and therapists, ENT specialists, child psychologists and counselors as well as family support groups played little part in the treatment of children with cleft palates prior to and after surgery in the days gone by.
who wrote in 1983, that the main contributors that have revolutionized cleft palate surgery over the years more often than not do not contain representatives of the “speech world”. The statement riddled with a double negative, in plain words, points out that speech pathologists and therapists, ENT specialists, child psychologists and counselors as well as family support groups played little part in the treatment of children with cleft palates prior to and after surgery in the days gone by. - This chapter aims to inform the plastic surgeon about the help that he/she must take from these professionals and the circumstances which will indicate that such help is needed. The information about development of speech provided in this chapter is very brief and is not precise by the standards of a speech pathologist. Therefore two separate sections as addenda and comments are provided at the end of the chapter. The chapter also deals with those aspects of surgery which achieve a better length and function of the velum as well as secondary methods when the results of primary surgery are unsatisfactory. The primary repair of cleft palates has already been covered in the previous chapter which may need to be referred to while reading this chapter.
 The term ‘speech world’ is interesting in another context. In the child, speech develops by imitating those who speak. When nothing is heard, nothing is likely to be spoken. As in the world of the deaf silence breeds silence. No speech had developed in the curious case of the ‘wolf boy’ in India (Fig. 2) who was rescued from a pack of wolves amongst which he had survived. He could not walk but only crawled, made sounds from his throat, was grossly undernourished and ultimately died from multiple infections contracted from his new environment to which he had no answers in terms of acquired immunity. Environment therefore plays a crucial part in the human development particularly in the development of speech which is a highly developed skill in humans as opposed to animals.
The term ‘speech world’ is interesting in another context. In the child, speech develops by imitating those who speak. When nothing is heard, nothing is likely to be spoken. As in the world of the deaf silence breeds silence. No speech had developed in the curious case of the ‘wolf boy’ in India (Fig. 2) who was rescued from a pack of wolves amongst which he had survived. He could not walk but only crawled, made sounds from his throat, was grossly undernourished and ultimately died from multiple infections contracted from his new environment to which he had no answers in terms of acquired immunity. Environment therefore plays a crucial part in the human development particularly in the development of speech which is a highly developed skill in humans as opposed to animals.- The plastic surgeon who sees the child immediately after birth and later continues to remain in touch with the family is in a good position to judge as to how the family is coping with the problem. In addition to reassuring the family in general, he must also tell the parents particularly the mother to communicate with the child by talking and creating an ‘auditory’ environment. The act of feeding is considered an important part of communication including the gestures and expressions that form a part of the feeding process. A distraught and therefore a somewhat dysfunctional mother may need a referral to a family group or a counselor.
- Babies with cleft of the palate take longer to feed, are prone to wind and this leads to disruptions in the feeding schedule. The air swallowed with the feed means the child must be held by the mother in the upright position, induced to burp and the burping may be accompanied by regurgitation of milk and bouts of cough. The surgeon (and the pediatrician) must warn the mother of this sequence and told to develop patience. These disruptions may mean that the child’s and the mother’s sleep schedules maybe disturbed. The surgeon at all times must listen to the mother’s woes in full and advise her to show patience and reassure her that these are passing phases and the final outcome will be satisfactory and if possible give examples of grown up children who have had surgery for cleft palate to demonstrate what can be achieved.
- For reasons not yet fully known the cleft palate child is vulnerable to serous middle ear effusion though it has something to do with the origin of the two extrinsic muscles of the palate, namely, the levator and the tensor palati which arise from near the openings of the Eustachian tube in the roof of the pharynx. The closure and the opening of this path into the middle ear is therefore disturbed due to the abnormality of the muscles in babies with clefts of the palate leading to ingress of unwanted material into the middle ear. This condition can be painful and is the second commonest cause of unexplained crying in infants, the commonest being gastrointestinal colic. When the condition is bilateral partial deafness may ensue which affects development of speech. The surgeon must be aware of this situation and an ENT examination followed by drainage of the serous fluid and introduction of gromets go a long way in both preventing pain, reducing intermittent deafness of long duration because this condition can be cyclical leading to better outcomes of speech.
- Recurrent nasal obstruction by colds or by the inherent nasal deformity in clefts of the lip accompanying clefts in the palate in which the septum is deviated to the normal side in the lower half of the nose can lead to mouth breathing, some snoring and disturbance of sleep. Nasal breathing is crucial to the development of the child and its absence does not exactly lead to retardation but certainly affects normal sequential growth and therefore can affect development of speech. The cleft of the lip therefore should be not only repaired as early as possible but some steps might be taken to centralize the septum to reduce nasal obstruction.
- Speech consists of phonation (sound) from the larynx, resonance around the pharyngeal space and later in the nose and the mouth aided by the para-nasal sinuses. All this helps in the formation of vowels. Consonants are created by a more designed neuromotor activity between the tongue, teeth, lips, the hard palate in front and the back, the soft palate and the glottis. This is called articulation. The gurgling or cooing of the normal new born infant at around the age of two months, a source of such joy and wonder to the parents is in fact an unconscious and involuntary attempt at vowelisation. With passage of time comes babbling where a consonant (or sometimes called contoid) comes to be created. For example, the sound ‘b’. But this can only happen when intra-oral pressure can be built with the help of the soft palate which rises to touch the posterior pharyngeal wall (Fig. 14) and the air can stream out with some pressure out of the mouth with intermittent closure of the lips and various movements of the tongue, for example bilabial consonants. This cannot happen when air escapes from the cleft of the palate through the nose. Please see addenda at the of the chapter.
- The international phonetic alphabet recognizes a series of basic consonants as well as their minute variations. Basically they consist of plosives, ‘b’ as in a boy. Dental sounds, ‘th’ as in thorium. Fricatives when friction is generated as in letters ‘s’ or ‘sh’; for example, sing, shoot or shrink. Approximation by the tip of the tongue to the hard palate creates ‘t’ as in Tom. The velar consonant sound such as ‘k’ as in king is produced when the tongue and the velum touch each other. A consonant such as ‘h’ is produced in the para-glottic area as in ‘Henry’ or ‘hound’. The consonant ‘ch’ as in ‘change’ is called an affricate (please see addenda at the end of the chapter).
- The development of consonants in a normal child is usually denoted by a term called ‘fronting’ to indicate that vowelisation from the posterior part has now progressed forwards. What begins as babbling progresses or ‘fronts’ to consonants. Words, some sort of sentences and a rudimentary language follow by the age of three years.
- In the older child for example of about four years with an untreated cleft palate and with normal hearing and IQ as well as a normal family, attempts by the child to imitate words spoken by him or her do not produce the anticipated results of which the child is aware both from what it hears of its own speech and from the responses that are aroused in those who are listening to him. The child may react in more than one way in this situation. It might stop communicating altogether or try to create consonants by shifting the position of the tongue backwards, called ‘backing’ to produce a zone of positive pressure in the pharyngeal area and try to articulate consonants in the best way possible. This might be accompanied by snorts, naso-facial grimacing, abnormal resonance, audible nasal airflow and secondary changes in the quality of laryngeal voice leading to hoarseness. This can lead to frustration because of the realisation that he or she is failing to convey thoughts and cause serious psychological problems. However it is also amazing that many of these children overcome this situation and try to lead as normal a life as they can in spite of the unsatisfactory speech. This scenario is now less and less prevalent even in developing countries except in some of their most backward parts because some form of palatal closure gets effected at least by the age of three years.
- What is surprising is that in children whose clefts have been treated in time even as early as four to six months normal speech does not follow with the same speed and efficiency as compared to normal children though it is well documented that by the age of seven years nearly 60-70% of the operated children will have some form of intelligible speech without any help such as speech therapy notwithstanding some mild deafness following serous otitis media. The reasons for this delay lie in the hugely complex mechanism by which speech is produced. For one, the abnormal position of the levator and tensor palati and their later normalization by way of surgery does not mean that their function will be restored immediately post-operative. The structures have been secondarily contracted in their abnormal position for several months (intra-utero as well) and take time to lengthen and function. The closure of the naso-pharynx by the elevation of the soft palate (Fig. 14) is not a “one go” and “absolute process” because some air is allowed to escape intermittently to achieve resonance and also to produce some specific consonants. The closure of the naso-pharynx is also aided by the reduction of pharyngeal space in both the lateral and anterior-posterior direction (see Fig. 15-18 and adjoining paragraphs). The coordination of the newly reconstructed palate and this pharyngeal contraction take some time to be perfected.
- Information given so far is to equip the cleft surgeon to recognize problems as they appear from the time the cleft is operated till a year and a half after surgery during which the parents are most likely to consult the surgeon. Even if speech development has progressed satisfactorily, the need for follow up visits should be impressed upon parents because language development is to follow in which the production of words is not enough but they must follow in a logical grammatical sequence at a reasonable rate which is age appropriate. If there is a marked incidence of distorted consonants, to give an example, words such as ‘do’, ‘two’, ‘zoo’, ‘shoo’, ‘chew’ or ‘jew’ are vocalized as ‘goo’ then an obvious inference can be drawn that the fronting of consonants mentioned earlier has not progressed and the tongue is staying back to produce a similar word with the help of creating a pressure zone in the para-glottic area with a ‘g’. If the ‘goo’ in the above example is not accompanied by nasality the situation is favourable because what is required is to physically demonstrate to the child how to use the tongue effectively. When distortions such as these are noticed, around the age of two and a half to three years, a speech pathologist (therapist) must be consulted forthwith. Habits die hard and need help and correction in good time. The speech therapists are also in a much better position to diagnose conditions such as attention deficit disorders, an abnormally hyperactive child, retardation, a dysfunctional environment within the family and the need to consult a child psychologist when required. Ideally in units dedicated to treatment of clefts a joint multi-disciplinary meeting is a norm and though such an arrangement may not be possible in all units, communications between the cleft surgeon and various specialists is of the essence.
- Children with operated cleft palates from the age of four years speak in a language which is best described as heterogeneous. An analysis of such speech will reveal a very wide spectrum from almost normal to a total absence of ‘fronting’ with the development of very few consonants in their correct form.
- At this stage or even earlier major disruptions such as,
- Uvular breakdown extending in the distal soft palate
- A large central fistula between the hard and the soft palate
- A post-alveolar anterior palatal fistula
will require the surgeon’s attention.
The first and the second will need to be re-repaired (the subject is dealt with in a subsequent chapter).
- For anterior fistulae a plate or an obturator is a good option because the closure is difficult on account of shortage of tissue and any repair by importing tissue can then be postponed so that speech therapy can progress. During this time the orthodontist can align the maxillary arch which will reveal the true nature of the deficit in the area of the fistula (Fig. 3,4,5).
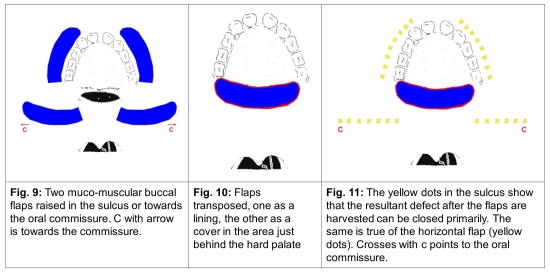
18. Prior to describing how to overcome naso-pharyngeal incompetence by surgical methods a brief description of the velar musculature which continues to be intriguing to the plastic surgeon is in order. These muscles are sometimes divided into two types. The intrinsic and extrinsic. The only intrinsic muscle of the velum is musculous uvulae which arises from the posterior edge of the palatine bone (spine) and traverses the whole length of the velum to the uvula but its function is not clearly known. Of the extrinsic muscles the tensor palati which occupies the anterior one third of the velum is hardly a muscle by the time it inserts in the posterior edge of the hard palate and is in fact only an aponeurosis with some stretchability. Because of its aponeurotic nature when a cleft forms it is shortened considerably, appears only like a tendon after it has gone around the handle of the hamulus and is extremely difficult to recreate when repairing a cleft. This then is the area of sorrow where in fact only the nasal and the oral layers of the velum get approximated at the time of the repair and it is in this area where fistulae form. Because the breadth of the tensor aponeurosis is not recreated in full, the palate may tend to remain short (Fig. 6). This predicament has resulted in several surgical procedures being described to overcome the shortage at the time of palatal repair. For example, the sandwich mucoperiosteal island flaps from the anterior part of the hard palate based on the greater palatine arteries (Millard), two long mucoperiosteal flaps from either side of the cleft in the hard palate, one as a lining and the other as a cover and the resultant large raw area later covered with a two stage tongue flap (Thatte) or two buccal muco-muscular flaps based posteriorly along the buccal sulcus flipped around the maxillary tuberocity, one flap as the nasal layer and the other as a lining. This flap can also be designed transversely from the molar to the oral commissure (Fig. 7-11). Recently a small turnover flap from the hard palate has been described by Sommerlad to compensate for the shortage in the central third of the tensor aponeurosis (please see previous chapter).
19. The restoration of the levator palati to its normal location in the central two thirds of the palate is comparatively easier because though lying in an abnormal vertical position, its muscular belly though probably secondarily contracted is easier to turnaround and is fully stretchable when adequately mobilized (please see previous chapter). Be that as may, that this newly reconstructed levator sling will not try to recoil to its original oblique position at least for some time till it finally settles down to its reoriented horizontal position cannot be guaranteed. The procedure such as a buccal flap which deters the recoil (mentioned earlier) (Fig. 10,11) or the Furlow Z-plasty (Fig. 12), ensures that such a recoil will be prevented. The unanswered question is, should such procedures be done primarily? As if to answer the question as this chapter was being compiled, Robert Mann of USA demonstrated in a long series of cases at the Chennai Smile Train conference in India September 4, 2015 in which a combination of Furlow’s Z-plasty in addition to buccal flaps, if required, were used in wide clefts with claims of excellent results.
20. Of the two tonsillar pillars the posterior one formed by the palato pharyngeous is stronger and is more important in narrowing the pharyngeal introitus. This narrowing is at a much lower level than the closure of the naso-pharynx which occurs at a higher level (at the level of the arch of the atlas) when the velum is pulled up by the action of the levator palati and it is this closure which is crucial to velo-pharyngeal competence. Also the palato-pharyngeous is an antagonist of the levator because it tends to pull down the velum as it pulls the posterior pillars medially. The narrowing of the pharyngeal introitus also aids in building up intra-oral pressure. It must be remembered that the velo-pharyngeal closure effected by the lifting of the velum at its shoulder with the uvula is intermittent in order to allow escape of air through the nose to allow it to acquire a resonant quality and this results from an intricate play between these two muscles, the palate-pharyngeous and the levator palati (Fig. 13,14). The superior constrictor muscle which encircles the pharynx in its posterior two third narrows the pharynx in the transverse axis as well as in the anterio-posterior direction. These actions also help in this complicated maneuver (Fig. 15-18). Please see next paragraph.
21. The superior constrictor in the throat by contracting reduces the total area of the naso-pharyngeal space, both laterally and anterio-posteriorly. After the advent of naso-endoscopy (please see para 23) it has been possible to see the normal closure of the naso-pharyngeal space and it appears that the commonest method of closure is coronal i.e. anterio-posterior in which the rising soft palate and the bulging posterior wall contribute. The next most common closure of the naso-pharyngeal space is concentric in which the lateral wall by way of contraction of the superior constrictor also helps in closing the naso-pharyngeal sphincter. The least common is the sagittal closure where only the lateral walls of the pharynx come together with some amount of the movement of the velum to close the naso-pharyngeal sphincter (Fig. 15-18).
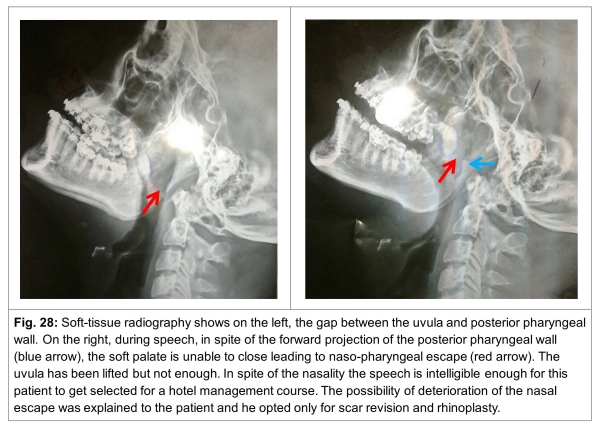
22. No fixed protocol which clearly states at what age treatment should be undertaken for nasopharyngeal escape is available because several units follow their own methods and some of them are personal and random. By the age of 5 years, if it is obvious that naso-pharyngeal escape is present causing difficulties in forming of consonants, treatment needs to be undertaken if it is found that the palate is very short and/or immobile on a simple oral examination. Soft tissue radiography as well as video fluoroscopy while the patient speaks will also be of great help to arrive at the diagnosis of naso-pharyngeal escape. Naso-endoscopy is difficult at this age. Of the possible solutions a re-pushback of the contracted soft palate and realignment of the levator palati, a buccal flap, or a Furlow’s z-plasty is undertaken by many units (see para 18-19 and accompanying figures). By the age of 8 years when speech continues to be unsatistactory in spite of speech therapy, a stage can be said to have been reached which goes by the name of ‘end stage velo-pharyngeal incompetence’. Here too though nasality may persist, but the speech is intelligible and the consonants are well formed, a more conservative non-surgical waiting period remains an option. But a combination of nasality and poor ‘fronting’ or negligible formation of consonants means that all attempts must be made to reduce the naso-pharyngeal escape to help the child improve speech. This can be done by any of the three procedures mentioned in para 18 and 19. There are no hard or fast rules as to how long the soft palate should be at eight years of age. If these procedures fail to improve the situation a pharyngoplasty is in order (see para 24 and figures 21 and 22). Some surgeons might opt to do a pharyngoplasty without interfering with the existing soft palate.
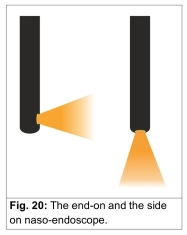
23. Ron-Piggot from Bristol (Fig. 19) was one of the first to successfully employ naso-endoscopy to diagnose the  nature of velo-pharyngeal incompetence. What began with a rigid naso-endoscope has now been mostly replaced with a flexible endoscope carrying light with the help of optical fibres. The view as obtained by the scope needs to be from above as well as ‘side on’. The view from above is ideal to see the movement of the lateral pharyngeal wall, while the ‘side on’ lateral view is best to judge the anterio-posterior movement both of the soft palate as well as the posterior pharyngeal wall (Fig. 20).
nature of velo-pharyngeal incompetence. What began with a rigid naso-endoscope has now been mostly replaced with a flexible endoscope carrying light with the help of optical fibres. The view as obtained by the scope needs to be from above as well as ‘side on’. The view from above is ideal to see the movement of the lateral pharyngeal wall, while the ‘side on’ lateral view is best to judge the anterio-posterior movement both of the soft palate as well as the posterior pharyngeal wall (Fig. 20).
 The diagnosis of the nature and location of deficiency ideally should determine the nature of surgery that needs to be performed. Here again as stated in the earlier paragraph should a diagnosis of a rigid and short soft palate be made, procedures such as the introduction of a buccal flap at the junction of hard and soft palate or a Furlow’s z-plasty might be considered as an option. If not, and when the soft palate appears adequately mobile but short and the discrepancy has as much to do with a deep pharynx, surgery involving the pharyngeal tissue is in order.
The diagnosis of the nature and location of deficiency ideally should determine the nature of surgery that needs to be performed. Here again as stated in the earlier paragraph should a diagnosis of a rigid and short soft palate be made, procedures such as the introduction of a buccal flap at the junction of hard and soft palate or a Furlow’s z-plasty might be considered as an option. If not, and when the soft palate appears adequately mobile but short and the discrepancy has as much to do with a deep pharynx, surgery involving the pharyngeal tissue is in order.
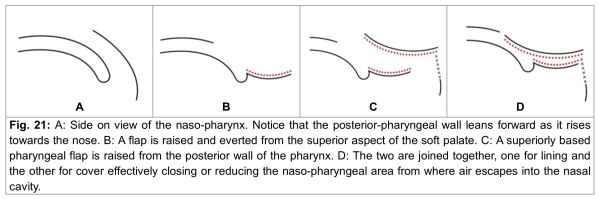
24. Pharyngoplasties are mainly divided into two types. In one, a muco-muscular flap from the posterior-pharyngeal wall is lifted and hitched on to the soft palate. This flap might be based superiorly (Fig. 21) or inferiorly. This procedure effectively reduces the pharyngeal space and it is doubtful if it has any dynamic action notwithstanding the inclusion of fibres of the superior constrictor. When it is based superiorly its blood supply is suspect because the vessels run from below upwards. In the event this flap is known to shrink and shrivel.
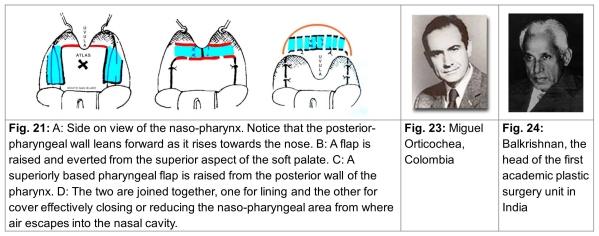
The inferiorly based flap is less popular because it weighs down on the soft palate. The other type of pharyngoplasty uses either the palate-pharyngeous (the posterior pillar of the tonsil), (Orticochea; Fig. 22 and 23) or the tissue on the lateral pharyngeal wall (Hynes, British plastic surgeon). Both these flaps are superiorly based and then are turned and sutured to the posterior pharyngeal wall by making either a transverse incision or raising a small flap on that wall. It has been argued that both these flaps contain muscular tissue and create an active muscular sling. The closure of raw area from where the flaps were harvested also narrows the pharynx. These flaps are also superiorly based and therefore their blood supply is suspect. It is not known whether they actually function dynamically or end up producing a tenodesing effect reducing the dimensions of the naso-pharyngeal area. It has also been debated if the tethering and antagonistic effect of the palato pharyngeous comes to be eliminated when such a flap is raised leading to a freer upward movement of the velum (Fig. 22). In this connection an operation described by Balakrishnan (Fig. 24, India) in which the tendon of the palmaris longus was used in the deep sub-mucous plane high up in the naso-pharynx to narrow that space needs to be mentioned.
- There are not enough data in numbers in the literature to show that pharyngoplasties specifically tailored according to the actual defect diagnosed by naso-endoscopy have worked better than a single method (for example the superiorly based pharyngeal flap) when it is employed for all cases irrespective of the nature of the defect. Many surgeons employ a single method of the above three and present anecdotal evidence of improvement. A pharyngoplasty is frequently undertaken without a naso-endoscopy.
- The above situation has led to attempts to create a bulge in the posterior-pharyngeal wall either with implants or autogenous tissue to reduce the naso-pharyngeal escape. Of the latter, reports on cartilage or fat injection have appeared in literature but grafts of fatty tissue tend to reduce by absorption and need to be reinjected. Cartilage is more durable but may migrate or rarely extrude. The same applies to implants perhaps with greater frequency. The data available in this regard are not large enough to come to any conclusions.
- Many patients with cleft of the palate with or without clefts of the lip will show deficient development of the maxilla with retrusion and poorly aligned maxillary and mandibular teeth and a somewhat flat appearance on the profile view. Maxillary advancement can solve the problem but there is evidence (from 10 to 50 percent in some series) that this procedure might lead to naso-pharyngeal escape and lead to deterioration in speech. The patient should be advised of these facts and only then should surgery for maxillary advancement be performed.
| Orthodontia and orthognathic surgery for patients with cleft lip and palate are covered in subsequent chapters. |
- All in all, though understanding of the problems about speech in patients with cleft palates has increased and the participation of allied specialities has improved results the surgeon around whom the treatment revolves is unable to prognosticate with any amount of certainty about the results that he will be able to achieve as far as speech is concerned. To be fair to the surgeon it must be stated that the environment in which the child grows, the child’s intelligence quotient, a certain degree of deafness, the difficulties of regular follow ups including inadequate speech therapy, all contribute to the final result which might be unsatisfactory. To use a modern expression, the “burden of care” imposed on the families with babies with clefts is huge and they are truly unable to cope with everything that is asked for by healthcare professionals. It also doesn’t help that both the upper and the lower jaw maybe deformed and particularly in the upper jaw abnormal dentition and deformities, both inherent and because of post-surgical scarring can contribute to less than satisfactory results because of difficulties in production of consonants.
Acknowledgments: Information given in this chapter comes mainly from the book, ‘Management of Cleft Lip and Palate’, ed. Watson, Sell and Grunwell, Whurr Publishers, 2001 and from Millard’s ‘Cleft Craft’, Little Brown & Company, 1980. Some of the illustrations in this chapter have been borrowed from these books and have been photoshopped for convenience.
Addendum:
ACH Watson, the international editor of these short notes and a co-author of one of the books mentioned above writes, “It does seem a shame that, nearly 20 years since I retired, we seem to be no nearer discovering which surgical technique might be best for the individual patient with speech problems. In the 1990s we had great hopes that multicentre trials and standardized recording methods should solve the problem. Alas it does not seem to have happened and the choice of treatment remains the individual surgeon’s own, based on his/her prejudices.” He hopes that better inter-centre collaboration with proper protocols gives us some answers in the future.
A critique by: Mrs. Aarti Pushkar Waknis
Associate Professor, Bharati Vidyapeeth University’s School of Audiology and Speech Language Pathology, Pune.
Para 2. Speech pathologist or therapists are alternative terms applied to the same healthcare professionals who deal with problems with development of speech because of a variety of causes. This critique is specific to this chapter. The numbers to the left refer to the paragraphs in the chapter.
Para 5. Under ideal circumstances, a speech therapist should be present at the time of the first interaction between the surgeon and the parents of the affected child. The therapist can help parents to “tune in” to the sounds that the child will make over time, advise them on how language develops and also helped them with problems regarding feeding.
Para 8. Nasal obstruction when severe will cause hyponasality and if accompanied by a severe velopharyngeal insufficiency will lead to a cul de sac resonance. Both will lead to a decrease in intelligibility and acceptability of speech.
Para 9. Articulation includes both vowels and consonants. Vowels are produced when a vibrated air column enters the oral cavity from the larynx and when subtle changes are made in the oral cavity mostly by the tongue, by its position as well as the height it assumes. The position of the lips is also important in these oral changes. Consonants on the other hand are produced when the tongue touches specific intra-oral parts such as teeth, the alveolar ridge, hard palate or the velum. The elevation of the velum and the closure of the naso-pharyngeal sphincter or the lack of it determines the nasality in the sound that is produced. In certain sounds such as ‘p’, the vocal cords are at rest. These are called unvoiced consonants. The bi-labial sound as in ‘b’ is however accompanied by a vibrating vocal cord and is therefore called ‘voiced’. Additionally sounds such as ‘th’ as in ‘theatre’, involve considerable egress of air and are called aspirated consonants. The letter ‘त’ a softer version of ‘th’ is typical of many Indian languages and is missing from English for example as in ‘Tendulkar’, the first ‘t’ is soft. These are called unaspirated consonants and have little movement of the vocal cords when articulated. That so many different sounds are produced leading to words and language and that they then assume a certain meaning requires precision and a coordinated sequential activity involving respiration, phonation, resonance and articulation is a wonder of the evolutionary process. In children with clefts, there may be both a delay and deviance from normal when consonants are produced.. This may be because of the abnormal altered anatomy or a failure to follow the rules of phonology (i.e. rules governing the production of speech sounds, please see a later paragraph). In addition to problems with articulation a delay both in comprehension of language as well as its expression is frequently noted in children with clefts. Babbling for example as in ‘ba, ba, ba’ or ‘da, da, da’ may appear late instead of the normal at about six months. The production of a meaningful set of words may also be delayed and this difficulty may persist up to three to five years.
Para 10. The International Phonetic Alphabet (IPA) is a system of symbols for representing sounds as well as accents (diacritics). This system helps to represent both normal as well as deviant speech sounds due to a variety of clinical conditions across global languages. Some sounds might be unique to a particular language and therefore its orthography (spellings and their correctness) may be different. The IPA can overcome these diacritical and orthographic difficulties. In languages such as Marathi and Hindi in India derived from Sanskrit, in which the alphabet is uniquely arranged phonetically.However some sounds such as glottal stops (where ‘papa’ is pronounced as ‘aaaa’) or pharyngeal fricatives cannot be represented using the standard orthography. The symbols in the IPA are a great help here.
Para 11. Visible sounds are those where the movements around the oral cavity when sounds are produced are more pronounced. There are other sounds which get generated without such movement and are called invisible. In the developing child the visible sounds/consonants are produced earlier. This goes by the name of ‘rule based phonological development’. Language is also developed in a certain sequence for e.g., a word gets structured (morphology), it gets related to its meaning (semantics), what follows is a certain syntax (as in grammar) to form a sentence. Under normal circumstances at the age of 3 years the child will be able to describe an event, tell a story or sing a nursery rhyme. The baby even with a repaired cleft may be late in this respect and will require help by a speech therapist.
Para 12. The backing of sounds in fact, in a way, break the rules of phonology and create several abnormal sounds as a compensatory mechanism and need to be corrected as soon as they are detected. The speech therapist can educate the parents in this regard while he/she continues to give therapy like in a tuition which can be replicatedby the parents. It is now universally accepted that surgery before one year leads to better outcomes of speech.
Para 14. In addition to the first consult after birth as mentioned earlier, the child will benefit a great deal if the speech therapist can meet with the parents after surgery on the palate so that they can be appraised of the sequence of production of various sounds, words as well as language. Should deviant sounds start appearing, they can be advised on taking preventive/ corrective measures with the help of the therapist.
Para 22. Intervention by a speech language pathologist will help in the management of delayed language development and compensatory errors. However, therapy will not work for correction of the obligatory errors andmore than mild hypernasality. These will require either surgical correction or prosthetic management, for example, a speech bulb which blocks the naso-pharyngeal space without adversely affecting breathing. Speech should be ‘normalized’ ideally before the child enters formal schooling or it may interfere with the process of reading and thus writing and also affect the social and emotional development of the child.
Para 27. Some techniques of maxillary advancement are being developed in recent years wherein the posterior portion of the palate (soft palate) is left undisturbed, thus preventing an increase in velopharyngeal in sufficiency when present. Orthodontists or surgeons could discuss these options with the patients and their families.
Sonakshi Rawal (Consultant Speech Language Pathologist and Audiologist, Godrej Memorial Hospital (Smile Train NGO), writes the following comments on this chapter.
The nasal, oral and pharyngeal features are very important in the development of speech and resonance and unfortunately these are the ones affected in individuals with cleft palate. The physical stigma and social stigma that are associated with a cleft of lip and/or palate require management by professionals. Speech and language therapy play an important role in the management of individuals with cleft of the palate. In addition to surgical and orthodontic management, difficulties with speech and language, difficulties in feeding, hearing problems, psychological issues are some of the concerns that need to be addressed in individuals with cleft palate.
Parents of babies with cleft palate face feeding difficulties immediately after their child’s birth. Therefore an upright position for the baby is advised post-feeding so that the child can burp. For a baby with cleft of lip feeding may not be an issue but for one with a cleft palate the negative pressure required for sucking cannot be created in the oral cavity because air tends to escape through the cleft. Different types of devices like specialized nipples or feeding bottles are available for these infants. The plastic surgeon and the speech language pathologist (SLP) together advise the parent about feeding. The SLP instructs the parents regarding key oral motor facilitation techniques during the process of feeding, especially to reduce nasal regurgitation. Instrumental assessment of swallowing can also be done when feeding is difficult.
Children with cleft palate are at risk of a delay in the development of speech as well as and language, if not provided with early intervention and adequate stimulation. Children with craniofacial anomalies/syndromes are even at a greater risk. Environmental stimulation, parent child interaction, brain structure, motivation, attention and hearing play a crucial role in early language development of the child. Several authors state that children with cleft may have a delay in cognitive or prelanguage skills. (Cognition pertains to memory, response, attention, perception of information. Play skills, imitation of actions, attention, interaction are all pre cursors to language/linguistic development). Children with a compensatory articulation disorder (CAD) have more language delay than those without CAD. Difficulties in Early sound development like cooing, babbling may signify an expressive language delay and these are an important part of normal language development.
The infant with cleft palate lacks the positive pressure required to produce an oral sound thus resulting in nasal escape or nasalization of an oral bilabial /b/ for instance. As infants we all are spoken to with a different intonation and stress pattern, in a rhythmic form with simple words, this is called as child directed speech or ‘motherese’. Parents of babies with cleft palate must stimulate their child’s receptive and expressive language. Early intervention is essential to improve the child’s speech and language skills. When behavioral problems exist the child must be sent to a SLP who will evaluate language and also decide whther the child may have associated problems of attention, temper tantrums, behaviours issues etc. these children may also require some form of occupational therapy and parents may need psychological counseling.
Resonance relates to the modification of sound from the larynx. The height of the velum, the configuration of the pharynx are affected by the tongue position during the production of speech sounds. Resonance disorders and velopharyngeal dysfunction are seen in children with cleft palate. Resonance may be hypernasal, hyponasal, denasal, mixed resonance and cul de sac resonance. Nasal air emission, weak or omitted consonants, short utterance length, compensatory and obligatory articulation errors are some of the effects of velopharyngeal dysfunction (VPD) on speech. VPD may not always be due to a cleft but can also be due to adenoids, a short palate, high pharynx etc. In others VPD can be due to dysarthria (motor speech disorder) accompanied by muscle weakness, mislearning, cranial nerve defects, apraxia (motor speech disorder affecting planning, programming and execution of speech muscles). Motor speech disorders may have hypernasality affecting speech.
In addition to a cleft palate a hearing loss may also be present. A Eustachian tube dysfunction, anomaly of the outer ear, middle ear and inner ear could be some of the causes of a hearing loss. Therefore it is essential to evaluate hearing of an individual with cleft palate. A pure tone audiogram, Brainstem evoked Response Audiometry (BERA), Immittance Audiometry (IA) can be done to rule out a hearing loss. The auditory skills of a person with cleft palate should be closely observed and the person must be referred for a hearing evaluation if suspecting a hearing loss. This is because hearing can affect the child’s language and articulation skills to a great extent. The SLP also works closely with dental professionals to determine whether articulation errors are due to dentition or not, whether they are compensatory or obligatory and whether correction is required or not. Similary together with a prosthodontist, a prosthesis can be devised and speech is evaluated with and without the prosthesis. As active team members, adequate follow up, treatment timing, sequencing and efficient use of resource are essential to ensure the best outcomes.
SLPs carry out a detailed speech and language evaluation for individuals with cleft palate. An articulatory assessment, language assessment, aerodynamic assessment (if stated) and nasality assessment, Oro facial examination, language screening (can be done through a parent questionnaire), informal and formal language screening are done by the speech language pathologist. Speech samples are collected and recorded to apply formal articulation tests, perceptual evaluation, acoustic evaluation. A number of tasks like counting, syllable and sentence repetition, spontaneous connected speech, picture descripition are carried out. Nasal air emission, stimulability, voice evaluation are also done by an SLP. SLPs also use instruments to carry out evaluation, these may be a voice software to evaluate voice (eg. Multi Dimensional Voice Profile), nasometer to evaluate nasality. In addition to this a nasoendoscopy by a team of surgeons and SLPs must be carried out. During the endoscopy and nasometry, the most essential is the stimulus provided to the individual with cleft palate, this will determine the errors in speech. On the basis of the findings from evaluation SLPs devise a treatment plan for infants/toddlers/adults. These target articulation errors, language concepts, social interaction. Every 3-6 months SLPs re-evaluate the child/adult to determine the goals achieved and to determine the progress in therapy.
Speech therapy is effective in correction of articulatory errors and language difficulties. Therapy is almost always ineffective in correcting hypernasality. It is very important to determine the candidate for speech therapy. Therapy should be given as long as the child makes progress, if the child is not responding to therapy and continues to have VPI, it may require to be referred to a surgeon for further intervention.