39. Ankylosis of the Temporo-Mandibular Joint/joints (TMJ)
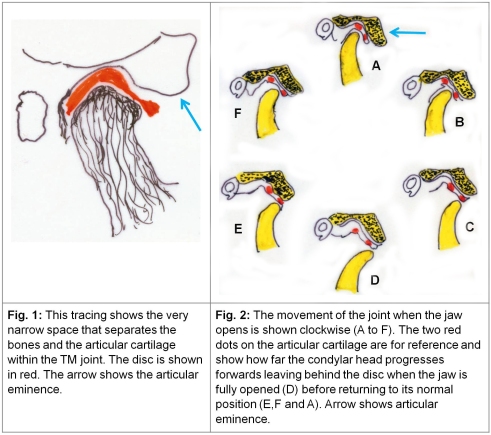
1. Anatomical peculiarities of the TM joint: The articulating elements in the TM joint, viz. the condylar head of the mandible and the fossa in the squamous part of the temporal bone form as two distinct bones. This is unlike a majority of the joints in the body which form by invagination within a single mesenchymal mass, which develops into two distinct bones and then gets covered by cartilage to form articular surfaces. In the event the articular disc within the TMJ is a unique structure in that it is this disc which articulates with the temporal bone above and the condylar head below (Fig. 1). In fact the condylar head together with the disc glides forwards up to a point as the jaw begins to open and then moves forwards independently in relation to the disc beyond the articular eminence when the jaw opens fully (Fig. 2).
Notwithstanding its small size, the joint is subjected to enormous dynamic forces when a person chews, grinds and crushes food and except during sleep the joint is subject to almost constant movement, voluntarily while speaking and involuntarily when emotions affect the major facial muscles. The articular disc plays an important role in these movements and its health is crucial to the TM joint.
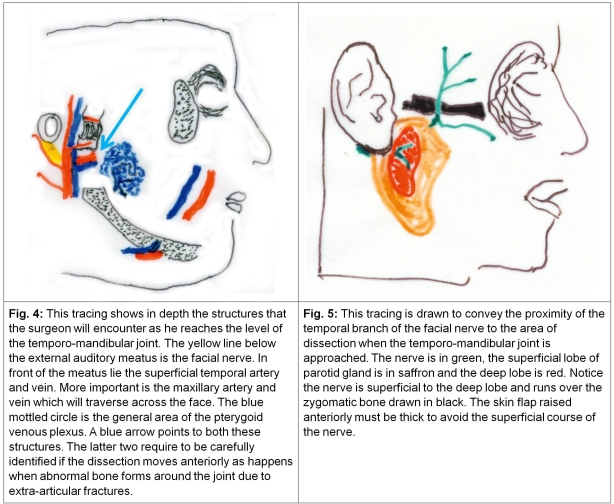
1a. Causes of TM Joint Ankylosis: The joint lies within a highly vascularised zone. The external-carotid artery ends by dividing into the superficial temporal and maxillary vessels in this area. Any injury which affects the articular disc leading to fragmentation and / or necrosis or a fracture high on the condyle or low on the temporal bone and an intra-articular haematoma exposes the joint to a vigorous osteogenic activity particularly in children. Deposition of new bone which straddles the mandibular and temporal bones leading to hypo-mobility or bony ankylosis. This matter is referred to in the chapter 37 on Fractures of the Mandible and it was stressed that injuries to the condylar head up to its neck need to be diagnosed precisely and then treated with some rest followed by physiotherapy. The area of the temporo-mandibular joint is crowded in that it has the external auditory meatus behind it, the coronoid process posterio-inferiorly and the junction of temporo-zygomatic bones superio-anteriorly (Fig. 3). Fractures of these bones are also likely to result in fibrosis/excessive bone formation leading to secondary hypo-mobility or extraarticular ankylosis of the TM joint and might require greater exposure for the removal of the abnormal bone (see Fig. 11).
The temporal branch of the facial nerve emerges from the parotid gland in this area (Fig. 5). This description is given because the most frequently employed incision to approach the temporo-mandibular joint is taken vertically in front of the tragus (Fig. 6) and is extended if necessary in the temporal area in the form of a hockey stick. When raising the skin anteriorly, care has to be taken to save the nerve which runs a subcutaneous course in this area and may be damaged. In more severe forms of extra-articular ankylosis dissection may extend deep into the area of the cheek where the maxillary artery as well as the pterygoid plexus of veins are encountered and can be a source of considerable bleeding if not identified (Fig. 4).
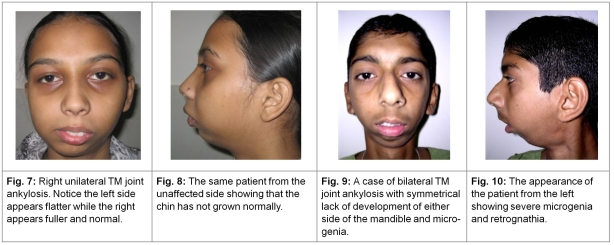
2. Pathologic anatomy and physical features of intra-articular ankylosis: Fractures involving structures close to the joint (high intra-capsular parts of the condyle with damage to the articular disc) more often than not occur in the first two decades of life and may influence growth of the mandible since the growing centre of the mandible is located in the condylar head. Also any hypo-mobility in the joint reduces muscular activity and something akin to disuse atrophy follows. When the ankylosis is unilateral, the normal mandibular side continues to grow and crosses the midline and the inter-incisor occlusion gets affected. The face appears longer and flatter on the normal side. The affected side is shorter in both its vertical and horizontal parts, the face appears crowded, the eruption of teeth is affected and in a clinical paradox the normal side may appear to be pathological at first inspection, till a more detailed inspection is carried out. When the ankylosis is bilateral, the deformed face, may be symmetrical but some degree of microgenia and / or retrognathia will be invariably present (Fig. 7-10). Attempts to open the mouth voluntarily or by external force fail even when the pathology is unilateral though some lateral movement as well as a protrusive effort on the normal side might be evident. Surprisingly the patients usually learn tricks to somehow imbibe liquid nourishment and are not always malnourished but are usually underweight. Dental hygiene is adversely affected.
Photographs courtesy Prof. Sanjeev Deshpande.
In the past severe infections in the area around the TMJ were a frequent cause of ankylosis and this was usually unilateral. Severe otitis media and mastoiditis, fulminating parotitis and secondary arthritis following haemorrhagic small pox caused destruction of the joint including the articular disc. These cases had extensive dense fibrosis around the destroyed joint as compared to bony ankylosis caused by an injury. This situation has now changed dramatically for the better even in India.
3. Surgical treatment: While approaching the TM joint by a pre-auricular incision, the superficial temporal artery is easily felt and should be marked prior to liberal infiltration with a saline adrenaline solution. This infiltration saves unnecessary oozing. The superficial temporal artery is saved as the dissection is deepened to the bony or fibrous pathology because it may constitute the source for a flap from the temporal area which might be used to line the defect created by excision of the pathological tissue (Fig. 3). The flap of skin and subcutaneous tissue is developed quite deep up to the level of the pathology and is extended anteriorly to expose the whole area of the fibrous and bony pathology. This will take care of the upper branches of the facial nerve (Fig. 5). If this pathology extends to the zygomatic arch, the hockey stick extension is then employed (Fig. 6).
That the surgical treatment of bony ankylosis of the TM joint must involve the removal of incriminated abnormal new bone is obvious but to that several riders need to be added for e.g.,
a. Cases of extra-articular bony ankylosis due to abnormal bone formation following fractures in the surrounding areas are a category by themselves. When the abnormal bone is removed a normal TM joint will be evident (Fig. 11-13) and vigorous post-op physiotherapy to overcome secondary soft tissue contractures needs to be followed. In these cases the contracted soft tissue for e.g. the temporalis tendon attached to the coronoid process gets cut during the surgical procedure and retracts. However the contracted deep temporal fascia which envelopes the zygomatic bone needs to be released transversely as a deliberate surgical step.
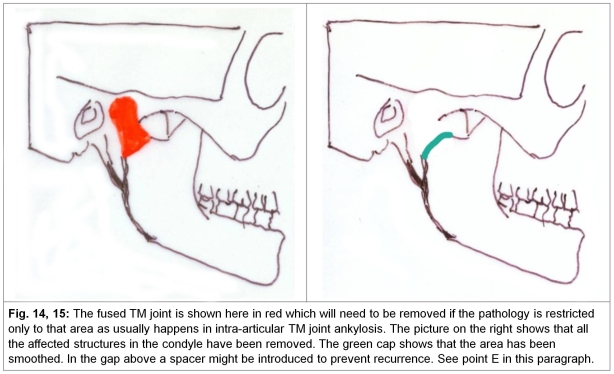
b. In ankylosis resulting from intra-articular pathology, the joint is destroyed and not only is it necessary to remove all incriminated bone but a thought has to be given to creating a surface, particularly on the condylar side, which will allow a joint-like movement (Fig. 14,15). When the procedure is undertaken in children, minimum but adequate bony excision needs to be undertaken to preserve the vertical height of the ramus. This is because the growth centre located in the condylar head is now extinct and the growth on the normal side will lead to severe imbalance if too much bone is excised. The options for reconstruction in cases of intra-articular ankylosis are given in a separate paragraph below. The secondary contracture in cases of intra-articular ankylosis is more likely to involve the masseter and its fascia and will need a deliberate and thorough release. Prof. Sanjeev Deshpande, head of Plastic Surgery of the NKP Salve Medical College, Nagpur, India who has a fair body of work on this subject to his credit and whose liberal help has been taken to draft this chapter adds that releasing the pterygomasseteric sling through a submandibular incision is necessary in addition to releasing the masseteric fascia and the temporalis fascia including excision of the coronoid process may be needed for a full release (See Fig. 1-3 in chapter 38 on Oral Submucous Fibrosis).
c. In both intra and extra articular ankylosis, acceptable levels of an oral opening may not be possible when surgery is completed in spite of clearing all abnormal bone as well as incising secondarily contracted soft tissue. In unilateral cases the secondary contractures on the normal side cannot obviously be treated with surgery and only vigorous post-op physiotherapy active as well as by mechanical appliances in the post-operative period are crucial for a good result. The appliances for achieving an adequate oral commissure have been shown with figures in the previous chapter on Oral sub-mucous fibrosis (see figures 13-16 in chapter 38: OSMF).
4. Methods of surgical treatment: In cases of intra-articular ankylosis following a post traumatic bony and cartilagenous injury a spectrum of solutions have been tried and are given below.
a. Several incisions have been used to approach the area, a bicoronal scalping incision from above, an end-aural incision or the pre-auricular incision curving like a hockey stick within the hair line above in the temporal region (Fig. 6). The last incision is perhaps the most frequently employed.
b. Removal of all abnormal bone and release of soft tissue leaving behind a gap followed by vigorous physiotherapy. Often the mandibular end is smoothed to resemble an articulating surface (Fig. 14,15).
c. Interposition of muscle or fascia or both within the gap created by removal of abnormal bone as a free graft or as a living flap from the temporalis muscle and fascia from the same side (Fig. 16-26).
Case report courtesy: Nisheet Agni, Mumbai
Case report courtesy: Nitin Mokal, Mumbai
d. Line the gap with free costochondral cartilage on one or both opposing excised surfaces viz. the excised condyle and the raw temporal bone. The cartilage is usually fixed with absorbable sutures (Fig. 27-30).
Case report courtesy: Prof. Sanjeev Deshpande
e. Interpose a part of the upper end of the fibula with its cartilage on the mandibular side as a peg (Fig. 35-37).
f. Use of materials such as silicon sheets, silicon blocks or even prefabricated non reactive metallic joints. This has been referred to in Fig. 14 and 15.
Pathologica curiosa
Nitin Mokal, craniomaxillofacial surgeon from Mumbai recently showed two unusual cases where not only did a fibular graft survive but grew even though it was a free graft (not a microvascular transfer) and overrode the TM joint though post operative mouth opening remained unaffected (Fig. 38, 39).
5. Anaesthesia: The subject of anaesthesia when the oral opening is very poor has been covered in the earlier chapter (chapter 38) on Submucous Oral Fibrosis. In adults, unilateral surgery on the temporo-mandibular joint can be done under local anaesthesia and sedation. Once the bony impediment is removed and the jaw is able to open to some extent it might be possible to induce general anaesthesia after an intra-tracheal intubation, and the release of the fibrosis surrounding the ankylosed joint can be undertaken in a thorough manner which is usually difficult under local anaesthesia alone.